Living with lupus means managing a complex and often unpredictable autoimmune condition that can affect many parts of the body. While medication and regular medical care are essential, lifestyle factors can also play a significant role in either stabilizing or exacerbating symptoms. Understanding the hidden lifestyle triggers that might worsen lupus is crucial for maintaining better control over the disease and improving overall quality of life. In this article, we will explore some of the less obvious habits and environmental factors that could be silently contributing to flare-ups, and offer practical tips on how to avoid them.
You think you’re doing everything right — taking your medications, resting when needed, trying to eat “healthy.” Still, your lupus flares come out of nowhere. What if the real culprit isn’t obvious? What if something as ordinary as your daily meals, sunlight exposure or stress is secretly feeding your lupus — and making you pay?
This may be the hidden truth many with Systemic Lupus Erythematosus (SLE) never hear about. In this post, we’ll unveil lifestyle and diet triggers often overlooked, explain why they matter, and show you a path toward better management and fewer flare-ups.
Why Lifestyle Matters for Lupus
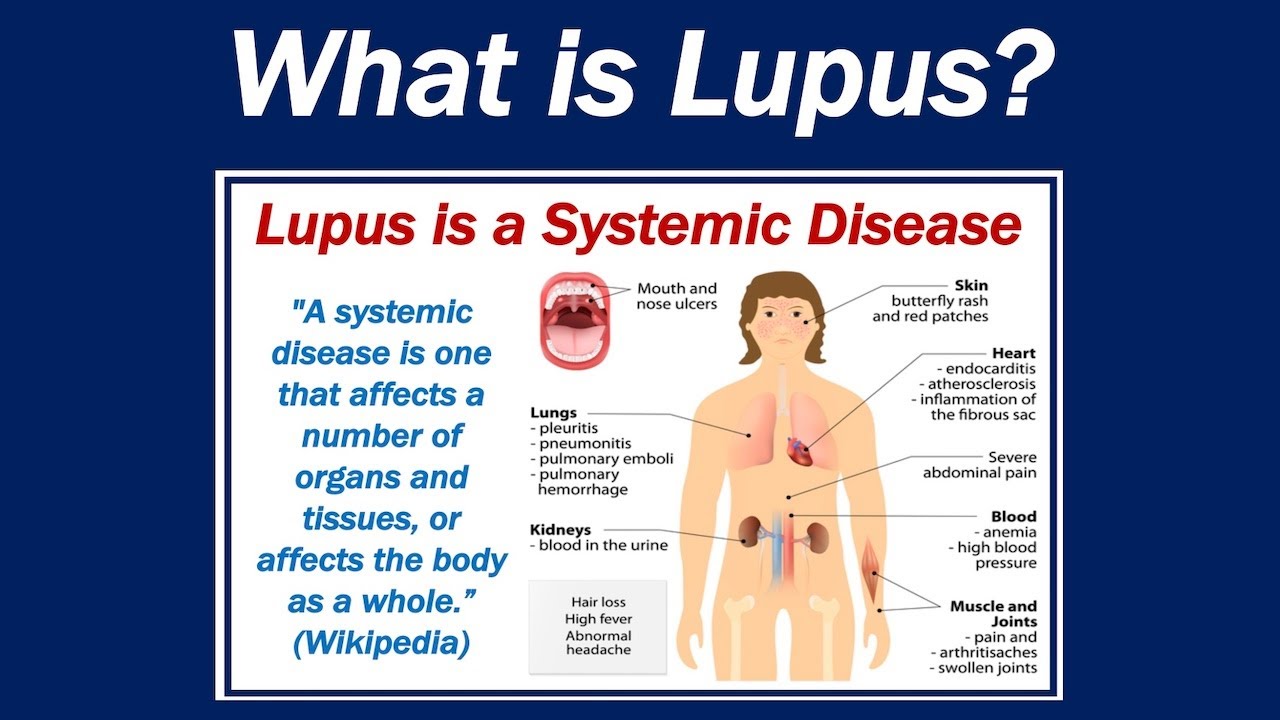
Lupus is not just some occasional joint pain or rash — it’s a chronic autoimmune disease. Your immune system mistakenly attacks healthy tissue, causing inflammation that can affect skin, joints, kidneys and more. (Office on Women’s Health)
Because inflammation lies at the heart of lupus flares, what you eat, how much rest you get, your stress levels, and your exposure to environmental triggers — all of it — can influence how intensely lupus hits you. (Healthline)
That’s why diet and lifestyle aren’t “extras” when you have lupus — they are essential parts of your wellness puzzle.
Common Lifestyle & Dietary Triggers for Lupus Flares
Here’s a breakdown of lifestyle and diet-related triggers that research and lupus-care experts frequently highlight. Because lupus affects people differently, not all triggers will hit everyone — but these are among the most commonly reported culprits.
| Trigger | Why It Matters / How It Affects Lupus |
|---|---|
| Sunlight / UV exposure | UV rays can provoke skin rashes, fatigue, joint pain, and full-blown flares in lupus sufferers who are photosensitive. Even artificial UV sources (fluorescent/halogen lights) may trigger reactions. |
| Stress, lack of rest, overwork | Emotional or physical stress, sleep deprivation and overexertion can stress the immune system and trigger flares. |
| Poor diet: processed foods, high saturated fat, high salt/sugar | These can promote inflammation, worsen fatigue, trigger flares, raise risk for heart disease or other lupus complications. |
| Immune-stimulating foods & supplements (e.g. alfalfa sprouts, garlic, certain herbs) | Some foods/supplements boost immune activity — which is dangerous in lupus, since the immune system is already overactive. |
| Smoking and exposure to toxins/chemicals | Tobacco smoke, certain chemicals, poor environmental exposures — all can aggravate lupus symptoms or trigger flares. |
| Skipping medications / treatment plan inconsistency | Stopping or mismanaging prescribed treatment can destabilize lupus and increase flare risk. |
Common “Hidden” Trigger Foods to Watch For
When it comes to lupus, some foods are innocuous for many — but for some, they may provoke flare-ups. Below are foods frequently flagged by researchers and lupus-care centers as potential problem-foods.
- Alfalfa sprouts (and alfalfa supplements): Contain an amino acid called L-canavanine which can stimulate the immune system and trigger inflammation, fatigue, or muscle pain.
- Garlic & certain immune-boosting herbs / supplements: While healthy for many people, in lupus, they may over-activate the immune system and cause flare-ups.
- Highly processed foods, fried foods, foods high in saturated fat, excessive salt or sugar: These can promote inflammation, worsen cardiovascular risk (many lupus patients already have elevated risk), and aggravate symptoms.
- Nightshade vegetables (for some people): While evidence is inconclusive, some people with lupus report sensitivity to nightshade vegetables (tomatoes, potatoes, peppers, eggplant), possibly due to their natural alkaloid compounds.
At the same time, certain dietary patterns seem to help — like a mostly plant-based, anti-inflammatory diet including healthy fats, lean proteins, omega-3s, fruits, vegetables, and whole grains.
Why Many Doctors Don’t Emphasize These Hidden Triggers — And Why That’s a Problem
- Lupus is unpredictable and individualized. Because lupus affects everyone differently, there’s no universal “lupus diet” or guarantee that a given trigger will affect all patients.
- Delayed or vague symptom onset. A flare might surface hours or even days after a trigger. That delay makes it hard to pinpoint cause.
- Many triggers overlap. Stress, poor sleep, sun exposure, diet, medication — often people are exposed to multiple triggers, so isolating one cause gets tricky.
- Lack of definitive, large-scale studies. While there’s considerable clinical guidance and patient observation, there’s limited large-scale, randomized research proving exactly which foods or lifestyle habits worsen lupus universally. Experts often give general recommendations for healthy eating rather than absolute restrictions.
Because of these factors, many doctors focus on medical treatment — sometimes neglecting deeper lifestyle counselling that could reduce flares.
How You Can Take Back Control: A Practical Lifestyle & Diet Strategy for Lupus
If you suspect lifestyle or food triggers may be contributing to your lupus flares, here’s what you can do. This isn’t about fear — it’s about empowerment.
✅ Step 1: Keep a personal flare journal
Record:
- What you eat (foods, portion sizes, timing)
- Your physical & emotional state — energy, mood, fatigue, joint pain, skin symptoms — over the next 24–48 hours
- Other factors: sun exposure, sleep quality, stress levels, medications, exposure to smoke/toxins
Over time, you may discover patterns — for example, joint pain after fried meals, or fatigue after sleepless nights.
✅ Step 2: Try an Elimination + Reintroduction Plan
Instead of permanently cutting many foods:
- Remove one suspected trigger food or habit at a time (e.g. alfalfa sprouts, or processed snacks).
- Wait 3–4 weeks and observe whether your symptoms improve.
- If symptoms ease, reintroduce the food carefully to test tolerance; if not, continue avoiding it.
This approach reduces unnecessary dietary restrictions while helping you learn what works for your body.
✅ Step 3: Embrace anti-inflammatory, nutrient-dense foods regularly
Include:
- Lean proteins: fatty fish (salmon, sardines), poultry, legumes
- Healthy fats & omega-3 sources: nuts, seeds, olive oil, fish oils (if approved by your doctor)
- Plenty of fruits and vegetables (especially leafy greens), whole grains, and calcium-rich foods for bone health — especially if you’re on medications like steroids.
✅ Step 4: Protect yourself from known triggers beyond food
- Sunlight / UV: Use high-SPF sunscreen, wear protective clothing, avoid sun during peak UV hours, consider UV-blocking films on windows.
- Stress, rest & sleep: Prioritize adequate sleep, take breaks, practice stress-reduction methods (meditation, gentle movement, hobbies).
- Avoid smoking, toxins, excessive alcohol: Smoking and chemical exposure are associated with increased lupus activity; alcohol can interfere with medications.
- Follow your medical treatment plan consistently: Skipping medications or altering treatment without professional guidance is a known trigger for flares.
Why This “Hidden Trigger” Strategy Matters — And Often Works
Because lupus is complicated — but partly manageable
You can’t control everything about lupus — genetics, immune dysregulation, organ involvement. But lifestyle is one area where you can make a difference. By tuning in to your body, being mindful about what you eat and how you live, you give yourself a better chance at fewer flares, less severe symptoms, and improved long-term health.
Because small changes add up
You don’t need a dramatic overhaul. Simple steps — journaling, swapping processed snacks for whole foods, wearing sunscreen — can slowly shift the balance from “what triggers me” to “what helps me.”
Because self-awareness helps you advocate for yourself
When you document symptom patterns and triggers, you’re not just guessing — you’re building evidence. That helps you communicate better with your doctor, tailor care to your needs, and avoid autopilot living where flares feel random and unmanageable.
Final Thoughts: Listen to Your Body — It Speaks If You Pay Attention
Living with lupus can feel like navigating a minefield — uncertain, fragile, full of potential triggers. It’s easy to feel powerless, especially when flares seem random.
But what if you could shine a light on some of those hidden triggers? What if your daily choices — what you eat, how you rest, how you manage stress — could shape how lupus affects you in the long run?
It won’t be perfect. Not everyone will respond the same. And you may not find all triggers quickly. But by treating your lifestyle and diet as part of your “treatment plan,” you give yourself a real shot at more stable, manageable days — and a calmer, more empowered life.
If you found this helpful — share it with someone living with lupus. And maybe, start your own flare journal today. 💙
Call to Action:
If this article resonated with you — share now with others who might benefit.
Thinking about starting a food & lifestyle journal for lupus — start today and discover your hidden triggers.
Want more lupus-friendly lifestyle insights?