fibroids are a common concern for many women, especially those trying to conceive. However, misconceptions and mistakes surrounding fibroid diagnosis and treatment can severely impact fertility and overall reproductive health. Understanding these pitfalls is crucial to avoid unnecessary complications and preserve the chance of pregnancy. In this article, we will explore some of the most unbelievable fibroid mistakes that are ruining women’s fertility and provide insights on how to navigate these challenges effectively.
What if everything you thought you knew about fibroids and fertility was wrong? What if simple mistakes — made even by well-meaning doctors — were secretly wrecking women’s chances of having a baby?
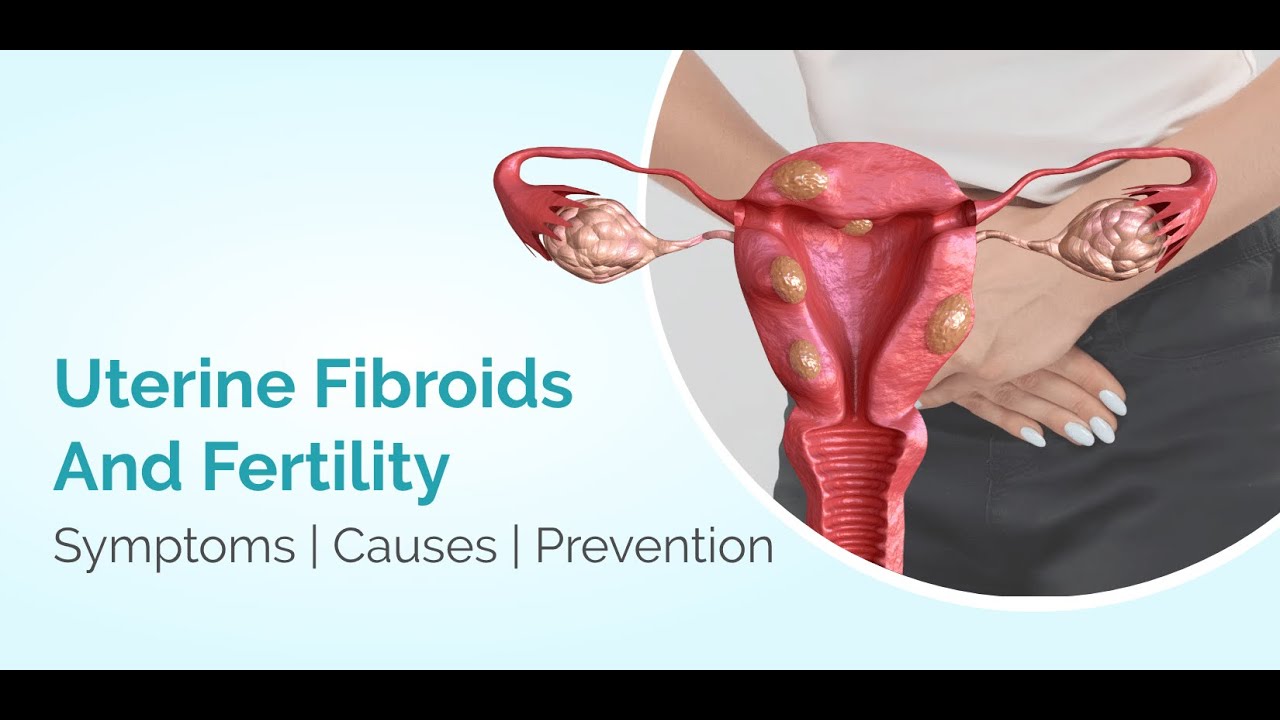
Uterine fibroids are one of the most common reproductive health conditions in women of childbearing age, but many people still don’t understand how they affect fertility — or how serious errors in diagnosis and treatment can make things worse. Today, we’re revealing the unbelievable fibroid mistakes that are quietly destroying women’s fertility — and what you must know to protect your reproductive future.
What Are Uterine Fibroids? (And Why They Matter for Fertility)
Uterine fibroids — also called leiomyomas — are non-cancerous muscle tumors that grow in and around the uterus. They affect up to 70% of women of reproductive age, though many are unaware they have them. (integration.reproductivefacts.org)
While fibroids often don’t cause symptoms, they can interfere with fertility — especially when they:
- Distort the shape of the uterus
- Block fallopian tubes
- Interfere with sperm or embryo movement
- Disrupt implantation of the embryo
According to fertility research, these impacts are especially strong when fibroids are located inside the uterine cavity (submucosal) or embedded deep in the uterine wall (intramural).
Yes — fibroids can be fertility killers, but only under the right (or wrong) circumstances.
Mistake #1: Ignoring Early Symptoms and Delaying Diagnosis
One of the most shocking errors women make — and doctors make too — is ignoring early signs of fibroids.
Many women assume painful periods, heavy bleeding, bloating, pelvic pressure, or prolonged bleeding are “normal.” But these can be red flags for fibroids and may significantly affect fertility if left unaddressed.
Numerous studies show that unnoticed fibroids — particularly submucosal ones that distort the uterine cavity — are strongly associated with infertility and difficulty conceiving.
Don’t wait — early detection matters.
Mistake #2: Misdiagnosis or Poor Screening Techniques
A surprising number of women go years without a correct diagnosis.
Poor imaging techniques or incomplete evaluations can miss fibroids that are affecting fertility. This means:
- Persistent fertility issues get incorrectly attributed to “unexplained infertility”
- Women undergo expensive and invasive fertility treatments that won’t work because underlying fibroids are the real problem
In fact, research shows that women whose fibroids distort the uterus have much lower pregnancy and implantation rates — and the odds improve only after proper diagnosis and treatment.
Best practice: Always insist on high-quality imaging (ultrasound, sonohysterogram, or MRI) if you suspect fibroids.
Mistake #3: Dismissing Fibroids as “Unrelated” to Fertility
Here’s one of the most unbelievable misconceptions out there: many clinicians still say fibroids don’t affect fertility — especially if they’re small.
That’s not true.
While not all fibroids cause infertility, growing evidence shows that submucosal and large intramural fibroids are strongly linked to reduced fertility and poorer reproductive outcomes.
It is possible to have fibroids and get pregnant, but dismissing fibroids outright — without understanding their location, size, or potential impact — can cost months or years of precious time trying to conceive.
Quick Fibroid Fertility Impact at a Glance
| Fibroid Type | Impact on Fertility | Typical Recommendation |
|---|---|---|
| Submucosal (inside uterine cavity) | High negative impact | Usually removed (hysteroscopic myomectomy) |
| Intramural (within wall) | Moderate — especially if >4 cm | Individualized plan; may need surgery |
| Subserosal (outside the uterus) | Little to no impact | Often just monitored |
Sources: Evidence summaries and clinical reviews.
Mistake #4: Choosing the Wrong Treatment Approach
Another unbelievable pitfall? Choosing the wrong treatment for fertility goals.
Many women — and some providers — still opt for:
- Uterine artery embolization (UAE)
- Hormonal therapy only
- Hysterectomy (uterus removal)
These may be appropriate in certain cases, but they can compromise fertility if used incorrectly.
For example:
UAE is not recommended when fertility is the goal, as it can damage the uterine blood supply vital for pregnancy.
Hysterectomy destroys any chance of natural pregnancy, yet it’s sometimes offered prematurely.
Leading experts emphasize that surgical removal of fertility-impacting fibroids (like submucosal ones) is usually the best choice when pregnancy is desired.
The key: Match treatment to fertility goals — not just symptom relief.
Mistake #5: Treating Without Understanding Location, Size & Symptoms
Not all fibroids are created equal.
Many women are treated based on size alone, or symptoms alone, without considering how location affects fertility.
For example:
- Two fibroids of equal size could mean very different fertility risks
- A small fibroid inside the uterine cavity may be far more problematic than a large one on the outer surface
Medical evidence shows that location is the top factor in whether fibroids impact reproduction.
The fertility battle isn’t against fibroids in general — it’s against the wrong action taken on the wrong type of fibroid.
Mistake #6: Waiting Too Long to Seek Specialist Care
Many women see a general practitioner or OB-GYN but never get referred to a fertility specialist.
This delay can cost time — and precious reproductive years — especially when:
- Trying for a pregnancy for 12+ months without success
- Age is over 35
- Multiple fibroids are present
Fertility specialists evaluate not just the presence of fibroids, but how they interact with your entire reproductive system — including ovulation, tube patency, and embryo implantation.
Mistake #7: Ignoring Emotional & Mental Toll
It’s easy to overlook just how devastating repeated fertility setbacks can be.
Women with undiagnosed or mistreated fibroids often:
- Feel isolated
- Experience anxiety and depression
- Blame themselves for infertility
- Encounter relationship stress
Fertility challenges aren’t just physical — they’re emotional too. Getting the right support matters.
Mistake #8: Not Preparing for Pregnancy After Fibroid Treatment
Many women think that once fibroids are removed, their fertility instantly returns to normal.
Not always.
After a myomectomy or surgical intervention:
- Healing time is essential before trying to conceive
- Scarring can still affect implantation
- Some women may still need assisted reproductive therapy
That’s why a personalized reproductive plan — developed with a specialist — is essential.
Conclusion: Knowledge Is Your Most Powerful Fertility Tool
Fibroids don’t have to sabotage fertility — but mistakes, misconceptions, and delays can make them feel like relentless obstacles.
Early detection
Accurate diagnosis
Fibroid type-specific treatment
Specialist involvement
Emotional support
…these are the foundations of fertility success in the presence of fibroids.
If you’re struggling to conceive, don’t settle for vague answers. Ask targeted questions. Get thorough imaging. See a fertility specialist who understands how unbelievable mistakes can silently sabotage your chances.
CTA:
If you found this article eye-opening, share it with a friend who’s trying to conceive — you never know whose fertility journey it might change.
Want more expert fertility insights? Read our next post on optimizing fertility after fibroid surgery.