Autoimmune diseases are on the rise at an alarming rate, affecting millions of people worldwide. Despite this growing epidemic, many are unaware of the hidden triggers that can ignite these complex conditions. From environmental factors to lifestyle choices, understanding these often-overlooked catalysts is crucial in managing and potentially preventing autoimmune disorders. the surprising triggers behind the surge in autoimmune diseases and explore what you can do to protect your health.
Autoimmune diseases are rising faster than almost any other chronic condition — and most people have no idea why.
What’s more disturbing is that many of the triggers are hiding in plain sight.
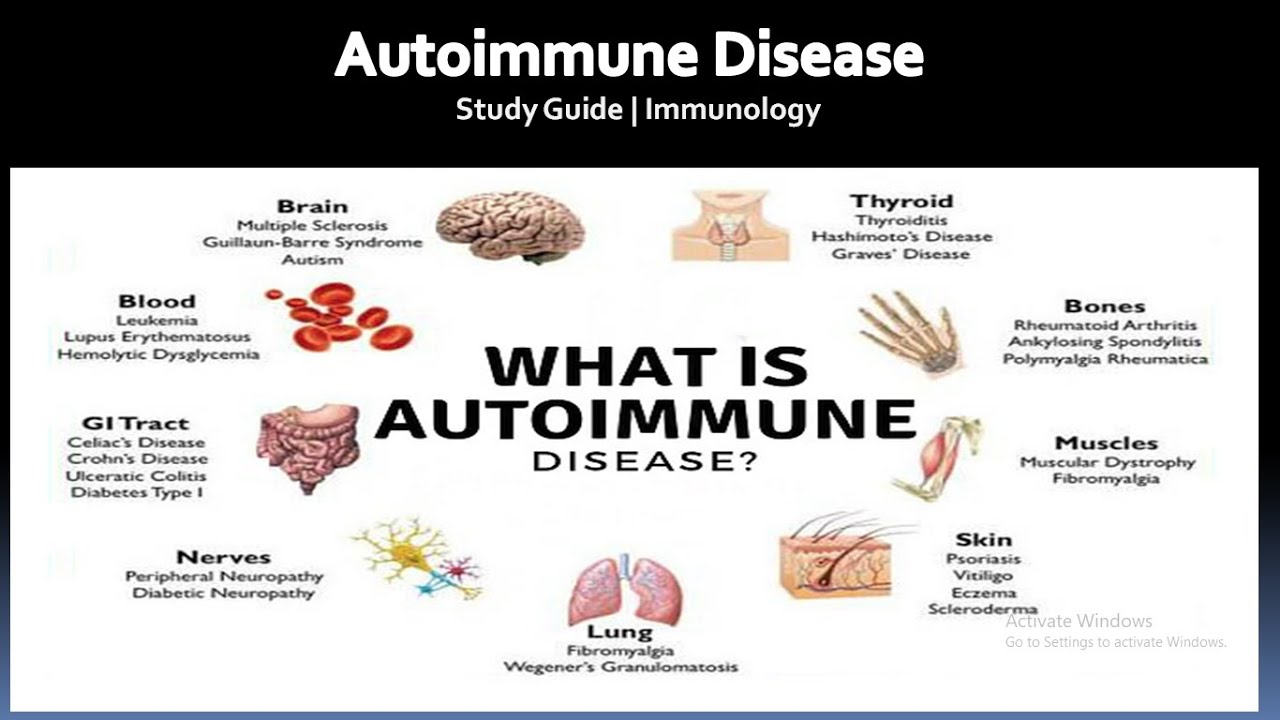
For decades, autoimmune diseases were considered rare. Today, they affect tens of millions worldwide, and diagnoses continue to climb year after year. Conditions like lupus, rheumatoid arthritis, multiple sclerosis, Hashimoto’s thyroiditis, and inflammatory bowel disease are no longer uncommon — they are becoming part of everyday medical conversations.
Yet despite this surge, many conversations stop at genetics or “bad luck.” That explanation is incomplete — and dangerously misleading.
As someone with decades of experience studying autoimmune conditions, one truth stands out: genes load the gun, but hidden triggers pull the trigger.
This article explores why autoimmune diseases are rising fast, the hidden triggers few doctors warn patients about, and what early warning signs deserve serious attention.
Why Autoimmune Diseases Are Rising Fast
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own tissues. While genetics play a role, genes alone cannot explain the sharp increase seen over the last 40 years.
What changed?
Our environment, lifestyle, diet, and stress levels.
Medical researchers increasingly agree that autoimmune diseases rise when the immune system is constantly overstimulated, confused, or damaged — often silently, over time.
According to large-scale epidemiological data, autoimmune conditions are among the fastest-growing chronic illnesses globally, especially among women and younger adults.
The Hidden Autoimmune Triggers No One Is Warning You About
This is where most people — and many clinicians — are caught off guard.
1. Chronic Stress as a Silent Immune Trigger
Stress isn’t just emotional. Long-term stress alters immune signaling, increases inflammation, and disrupts hormone balance.
When cortisol remains elevated for too long, the immune system can become dysregulated — attacking healthy tissue instead of pathogens.
Many patients recall autoimmune symptoms appearing after prolonged stress, such as:
- Job burnout
- Grief or trauma
- Caregiver fatigue
- Chronic sleep deprivation
Stress does not cause autoimmune disease alone — but it often activates it.
2. Environmental Toxins and Chemical Exposure
Modern life exposes us to thousands of chemicals our immune systems were never designed to handle.
Hidden triggers include:
- Pesticides and herbicides
- Heavy metals
- Air pollution
- Endocrine-disrupting chemicals in plastics
Research has shown that exposure to environmental toxins can provoke immune system malfunction, particularly in genetically susceptible individuals. This connection is increasingly documented in autoimmune research, including findings summarized by the National Institute of Environmental Health Sciences in its analysis of environmental autoimmune risk factors, which highlights how everyday chemical exposure may alter immune tolerance
https://www.niehs.nih.gov/health/topics/conditions/autoimmune-diseases-hidden-risks
3. Gut Health Breakdown and Immune Confusion
Roughly 70% of the immune system resides in the gut.
When the gut lining becomes damaged — a condition often referred to as increased intestinal permeability — immune cells may mistake food particles or microbes as threats.
Common contributors include:
- Highly processed foods
- Excess sugar
- Frequent antibiotic use
- Chronic inflammation
This gut-immune connection is one of the most under-discussed drivers of autoimmune disease onset.
4. Infections That “Flip the Switch”
Certain viral and bacterial infections can confuse the immune system through a process called molecular mimicry, where immune cells mistake human tissue for pathogens.
Infections linked to autoimmune activation include:
- Epstein-Barr virus
- Certain gut infections
- Recurrent untreated viral illnesses
Many patients report autoimmune symptoms beginning months or years after a “routine” infection that never fully resolved.
5. Hormonal Disruption — Especially in Women
Autoimmune diseases disproportionately affect women, particularly during:
- Puberty
- Pregnancy
- Postpartum
- Perimenopause
Hormonal shifts influence immune behavior. Estrogen, in particular, can amplify immune responses — sometimes tipping the balance into autoimmunity.
This partially explains why women represent nearly 80% of autoimmune diagnoses.
Hidden Autoimmune Triggers vs. Commonly Blamed Causes
| Commonly Blamed Cause | Hidden Autoimmune Trigger |
|---|---|
| “Just genetics” | Environmental toxins |
| Aging | Chronic immune stress |
| Bad luck | Gut barrier damage |
| Stress alone | Stress + immune dysregulation |
| Isolated infection | Persistent immune activation |
Early Warning Signs of Autoimmune Diseases Rising Fast
One reason autoimmune diseases continue rising is delayed recognition.
Early symptoms are often vague, dismissed, or misdiagnosed.
Warning signs include:
- Persistent fatigue that doesn’t improve with rest
- Joint pain or stiffness without injury
- Digestive issues that don’t respond to diet changes
- Brain fog or memory difficulty
- Unexplained rashes or skin changes
- Sensitivity to temperature or light
According to clinical insights summarized by Cleveland Clinic, autoimmune symptoms often develop gradually and overlap across systems, making early recognition critical for preventing progression
Why Doctors Often Miss These Hidden Triggers
Medical training traditionally emphasizes diagnosis after disease is fully expressed, not during early immune imbalance.
Challenges include:
- Symptoms spanning multiple systems
- Normal lab results in early stages
- Limited appointment time
- Over-reliance on single diagnostic markers
As a result, patients are frequently told:
- “Your tests are normal”
- “It’s probably stress”
- “Let’s wait and see”
Unfortunately, waiting often allows inflammation to deepen.
What You Can Do If You’re Concerned
While this article does not replace medical care, awareness is powerful.
Practical steps include:
- Tracking symptoms over time
- Requesting specialist evaluation when symptoms persist
- Addressing lifestyle inflammation (sleep, stress, diet)
- Reducing toxin exposure where possible
- Listening to your body — not dismissing it
Early action does not guarantee prevention, but it can slow progression and reduce severity.
Why Awareness Matters More Than Ever
Autoimmune diseases are rising fast not because people are weaker — but because modern life places unprecedented strain on the immune system.
The danger lies not only in the diseases themselves, but in the hidden triggers no one is warning you about.
When symptoms are brushed aside or triggers ignored, the immune system continues its silent attack.
Conclusion: The Conversation Must Change
Autoimmune diseases are no longer rare — and pretending otherwise costs people years of health, clarity, and quality of life.
Understanding hidden autoimmune triggers shifts the conversation from reaction to awareness. And awareness is often the first step toward better outcomes.
If this article resonated with you, it’s likely because you — or someone you know — has felt unheard.